Harvard Health Blog
Read posts from experts at Harvard Health Publishing covering a variety of health topics and perspectives on medical news.
Today’s ruling by the Supreme Court that largely upholds the Patient Protection and Affordable Care Act should be viewed as a landmark event—whether one agrees with it or not. The Supreme Court’s ruling means that many more people will have health insurance; that health care will continue to be provided largely by the private sector; and that insurance companies won’t be able to deny an individual coverage because he or she has a chronic medical condition, drop coverage if an individual becomes sick, or put limits on the amount of lifetime coverage a person can get. It also means that individuals without health insurance will have to pay for it, and that many employers who do not currently offer health insurance as a benefit will be required to do so, or pay a stiff penalty.
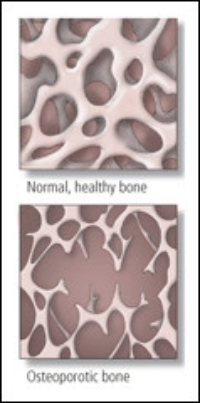
The U.S. Preventive Services Task Force (USPSTF) has stirred up a maelstrom of debate by proposing that healthy postmenopausal women lay off daily calcium and vitamin D supplements, which the task force says may do more harm than good. The USPSTF concluded that, based on the available evidence, supplements containing up to 400 IU of vitamin D and 1,000 milligrams (mg) of calcium don’t reduce fractures in postmenopausal women. Plus, these supplements may slightly increase the risk of kidney stones. As a result, the USPSTF says that postmenopausal women who aren’t at risk for osteoporosis shouldn’t be taking these supplements to prevent fractures. The jury is still out on whether it’s worth it for women and men to take higher doses of calcium and vitamin D to prevent fractures, or to take vitamin D to prevent cancer. Our experts say that most of your daily calcium should come from your kitchen, not your medicine chest.
We usually think of post-traumatic stress disorder (PTSD) as an aftermath of military combat or terrible trauma. It can also strike heart attack survivors. By the latest account, 1 in 8 people who live through a heart attack experiences a PTSD-like reaction that might be called post-traumatic stress disorder (PTSD). They experience the same key symptoms: flashbacks that occur as nightmares or intrusive thoughts. They try to avoid being reminded of the event and become hypervigilant worrying that it will happen again. As treatments for heart attack continue to improve, 1.4 million people a year are now surviving the event long enough to be discharged home. If the study is correct, 168,000 of them will be diagnosed with PTSD every year. It’s a grim reminder that as we get better at fixing the body, we must recognize the need to treat the mind.
Drinking alcohol during pregnancy has been taboo for some time, largely because drinking too much can cause fetal alcohol syndrome (FAS). Because no one has been able to identify a clear threshold for “safe” drinking during pregnancy, doctors tell women to steer away from alcohol entirely. A series of five studies from Denmark published in BJOG An International Journal of Obstetrics and Gynaecology found that “low” (1-4 drinks per week) to “moderate” (5-8 drinks per week) alcohol consumption in early pregnancy did not harm the neuropsychological development of children evaluated at age five. Drinking more appears to be a different story. In one of the studies, five-year-olds whose mothers consumed higher levels of alcohol (9 or more drinks per week) during pregnancy were significantly more likely to have lower attention spans. The authors of the study do not argue that drinking alcohol during pregnancy is wise or to be encouraged. In fact, most doctors will continue to advise pregnant women not to drink alcohol. is there a middle ground? Perhaps. Deciding to have a sip (or glass) of champagne at a special occasion during pregnancy may not be an unreasonable or unsafe choice–one that each woman has to make for herself, ideally after talking with her obstetrician or midwife about this issue.
Why is it so incredibly hard to quit smoking—even when you are desperate to do so? For some people, the answer may be in their genes. In a report published online in the American Journal of Psychiatry, a team led by Dr Li-Shiun Chen of the Washington University School of Medicine identified a “high risk” version of a nicotine receptor gene that is more common in heavy smokers. Those with the high-risk gene took two years longer to quit smoking. But there was a silver lining: smokers with the high-risk gene were three times more likely to respond to smoking cessation therapies. The study provides hope for even hardcore smokers. However long it takes, quitting is beneficial. In a study published in the Archives of Internal Medicine, quitting smoking reduced the risk of dying—even in people in their 80s. “Even older people who smoked for a lifetime without negative health consequences should be encouraged and supported to quit,” the researchers wrote.
For people who are obese, the operation known as gastric bypass surgery has been hailed as something of a miracle. In addition to rapid weight loss, it can reverse diabetes and reduce the risk of heart disease. A new study reveals potential darker side—an increase in alcohol abuse. In a presentation at yesterday’s annual meeting of the American Society for Metabolic and Bariatric Surgery, researchers reported that almost 11% of nearly 2,000 men and women who underwent gastric bypass surgery (the most common type of obesity surgery) got in trouble with drinking by the second year after surgery. About 7% drank too much before the operation, representing a 50% increase. This finding shouldn’t steer people who could benefit from gastric bypass surgery away from the procedure. But it should prompt them—and their doctors—to be on the lookout for changes in alcohol use or abuse afterward.
The idea that pain relief resides only in a bottle of pills is a common misconception. While medication often plays an important role in quelling pain, there’s a large arsenal of drug-free pain-relief therapies and techniques. The Institute of Medicine estimates that 116 million adults experience chronic pain each year. It has called for “a cultural transformation in how the nation understands and approaches pain management and prevention.” Improved pain management should include a combination of therapies and coping techniques. Other pain-relief therapies include biofeedback, ice, heat, exercise, acupuncture, hypnosis, massage, mind-body relaxation techniques, and more. These techniques can be used alone, in combination, and even in combination with drug therapy. Using non-drug therapies can be an empowering experience. Most of these therapies do not carry the risk of side effects as do most drugs. And many non-drug therapies are self-help techniques you can do by yourself or learn from a therapist.
The run-up to Father’s Day should be about more than ties, golf balls, and deciding what to grill on Sunday. Health should also be on the agenda. Men’s Health Week was created by the U.S. Congress in 1994 to boost awareness of men’s health and ways to improve it. It’s a good time for men to contemplate their vigor, fitness, and overall health—and then do something about it. Here are five things you can you do to improve your health. 1) Get moving. 2) Get checked for colorectal cancer. 3) Know your blood pressure. 4) Cut back on sodium in your diet. 5) Don’t ignore warning signs. This week, give yourself the gift of good health. And keep it going beyond Father’s Day.
Some encouraging Alzheimer’s news from Sweden: a vaccine called CAD106 appears to be safe and ramps up the body’s immune system against a protein likely involved in Alzheimer’s. The hope is that this vaccine will slow the progression of Alzheimer’s disease, and possibly even stop it. The vaccine is designed to activate the body’s immune system against beta amyloid, a protein fragment that forms deposits called amyloid plaques between nerve cells in the brain. Three-quarters of those who received CAD106 developed antibodies against beta amyloid protein. Virtually all of them—including those getting the placebo—reported one or more side effects, ranging from inflammation of the nose and throat to headache, muscle pain, and fatigue. None, though, developed meningoencephalitis, an inflammation of brain tissue that derailed work on an earlier version of the vaccine. The next step in the development of CAD106 is a larger clinical trial to confirm the vaccine’s safety and to see if it is effective at slowing the relentless progression of Alzheimer’s disease.
Fifty years ago this week, the first installment of Silent Spring appeared in the pages of The New Yorker. The book, published a few months later, was a sustained, meticulously reported account of the toll that widespread aerial spraying of DDT, dieldrin, aldrin, chlordane, heptachlor, and other synthetic pesticides was taking on birds, raccoons, fish, bees, and even the supposed beneficiaries of spraying—humans. Silent Spring is often portrayed as a book about saving birds and other wildlife. Another important theme is the essential but fragile connections between environmental health and human health. Silent Spring was instrumental in banning the use of many dangerous pesticides. It helped spark the modern environmental movement, launch the Environmental Protection Agency, and pass the Clean Water Act and the Endangered Species Acts. It is in the Modern Library’s 100 best nonfiction books, and Discover magazine named it one of the 25 greatest science books of all time.
Red meat hasn’t been getting very good press lately. Meat-heavy diets have been linked to increased risks of developing heart disease, diabetes, and some cancers. New findings from two long-term studies now indicate that eating lots of meat, especially processed meat, may also shorten your life.
Millions of people depend on the blood thinner warfarin to prevent clots from forming in their blood. It’s an important drug, but tricky to use. One problem with warfarin (Coumadin, Jantoven, generic) is that it interacts in potentially harmful ways with other medications. Two problematic types are antibiotics and antifungal agents. As we write in the June issue of the Harvard Heart Letter, this isn’t just a problem with pills, but can also happen with ointments, creams, and suppositories. Adding an antibiotic such as cotrimoxazole, cephalexin, or penicillin, or an antifungal medicine such as itraconazole or ketoconazole on top of warfarin can heighten warfarin’s blood-thinning ability. This raises the risk of internal bleeding or sustained bleeding after an injury.
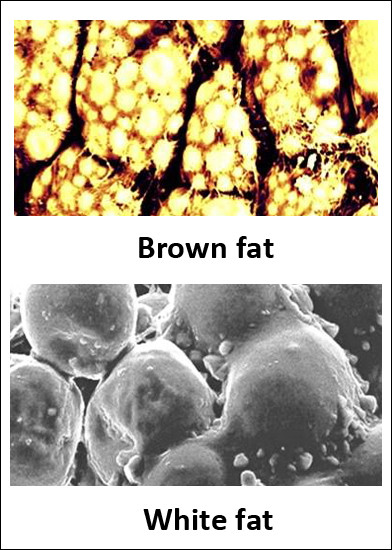
Exercise makes cells burn extra energy—that’s one way it helps control weight. It also generates a newly discovered hormone, called irisin, that transforms energy-storing white fat cells into energy-burning brown fat cells. Irisin also appears to help prevent or overcome cellular changes that lead to type 2 diabetes. The hormone does this by helping transform energy-storing white fat cells into energy-burning brown fat cells. White adipose tissue, more commonly known as body fat, is the tissue that dimples thighs, enlarges waists and derrieres, and pads internal organs. Each white fat cell stores a large droplet of fat. Brown fat, in comparison, is chock full of energy-burning mitochondria. Its main function is to generate body heat by burning fat. A team led by Dr. Bruce Spiegelman, professor of cell biology and medicine at Harvard Medical School, has identified irisin in mice and humans and showed how irisin transforms white fat cells into brown ones, at least in mice.
The symptoms of a stroke are sometimes obvious, like numbness or weakness on one side of the face, trouble speaking, difficulty walking, and vision problems. Some strokes, though, pass completely unnoticed—at least right away. But as reported in the June issue of the Harvard Women’s Health Watch, the damage these so-called silent strokes cause to fragile brain tissue can have significant and lasting effects on memory. Although silent strokes don’t cause any obvious symptoms, the interruption in blood flow to the brain can harm the processes needed to form or recall memories, especially if several of them occur over time. You can help prevent silent strokes the same way you others, by controlling blood pressure and cholesterol, not smoking, eating a healthy diet, and exercising.
Aspirin, ibuprofen, and naproxen can subdue a pounding headache and ease arthritic aches. Could these and other nonsteroidal anti-inflammatory drugs (NSAID) serve double duty, protecting against skin cancer even while they relieve pain? A new study published online in the journal Cancer suggests they might. But based on the current evidence, cancer prevention alone doesn’t justify downing NSAIDs and potentially exposing yourself to their side effects.
When you polish off a piece of chocolate cake and immediately start thinking about having another, you might suspect that eating for pleasure may trigger overeating. A new study out of Italy, where they know a thing or two about good food, supports this notion.
Calcium supplements are being called on the carpet after new research showed they significantly increased risk of heart attack among women getting extra calcium from pills, but not among those who got their calcium from food. What’s the connection? Over time, calcium can accumulate in arteries. It also builds up in plaque, the cholesterol-filled pockets that can cause angina or a heart attack. Three Harvard professors say the new study doesn’t prove that calcium supplements cause heart disease, but advocate that it’s almost always best to get vitamins and minerals from food, not pills.
When men in steady relationships contemplate their sexual woes, erectile dysfunction (ED) is usually at the top of the list. That’s understandable, since 20 to 30 million American men suffer from ED, and ads for drugs such as Viagra, Levitra, and Cialis carpet-bomb our consciousness of it in the media.
Every Memorial Day we remember the men and women who died while serving in the United States Armed Forces. We do this with parades, church services, and placing flags on graves. Another way to honor the fallen is by paying attention to the physical and mental health of those who served and returned.
Breast cancer isn’t just a woman’s disease. Men can get it, too—about 1% of breast cancer is diagnosed in men. Since few men know that, they often fail to recognize its earliest signs and end up seeing a doctor later in the process than women do. The result: Men face treatment for larger and more advanced tumors, and their cancer is more likely to have spread to other parts of the body. The largest study to date on outcomes in men with breast cancer indicates that the five-year survival rate for women with breast cancer was 83%, compared to 74% for men. Even men diagnosed with early stage breast cancer still fared worse than women, although the gap closed for men and women diagnosed with later-stage disease. Since breast cancer in men isn’t often on doctors’ radar screens, men should be aware and check themselves.
If you’ve battled bronchitis or endured an ear infection, chances are good you were prescribed the antibiotic azithromycin (Zithromax), which is commonly available in a five-day dose known as the Z-Pak. But a recent study suggests that the Z-Pak may do some harm even as it heals.
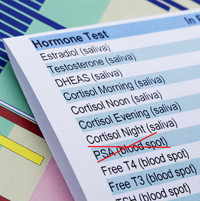
Yesterday’s announcement that men should not get routine PSA tests to check for hidden prostate cancer is sure to spark controversy for months to come. But the U.S. Preventive Services Task Force (USPSTF) made the right decision. On the surface, rejecting the use of a simple blood test that can detect cancer in its early and still-treatable stage sounds foolish. Cynics have been saying it is the handiwork of a group concerned more about health-care rationing and cutting costs than about health. The decision is wise, not foolish, and will improve men’s health, not harm it. The word “cancer” usually brings to mind images of a fast-growing cluster of cells that, without aggressive treatment, will invade other parts of the body, damage health, and potentially kill. That certainly describes many cancers. But not most prostate cancers. Most of the time, prostate cancer is sloth-like. It tends to grow slowly and remain confined to the prostate gland, with many men never knowing during their entire lives that a cancer was present. These slow-growing prostate cancers cause no symptoms and never threaten health or longevity. That means many men with prostate “cancer” never need treatment.
A simple blood test to check seemingly healthy men for hidden prostate cancer does more harm than good and shouldn’t be part of routine medical care. That’s the long-awaited final recommendation from the United States Preventive Services Task Force (USPSTF), published today in Annals of Internal Medicine. About half of men over age 40 get this test as part of a regular checkup. It measures the amount of a protein called prostate-specific antigen, or PSA, in the bloodstream. An above-normal PSA level can signal hidden prostate cancer. But it can also be a sign of prostate infection, an enlarged prostate, and other problems. Hunting for hidden disease in the absence of any outward signs or symptoms is called screening. The task force says that for every 1,000 men who have routine PSA tests, 0 to 1 deaths from prostate cancer will be prevented. But that is offset by 3 serious cardiovascular deaths due to treatment, along with 47 men who will live with treatment-related erectile dysfunction or incontinence.
Since bisphosphonates such as alendronate (Fosamax), ibandronate (Boniva), risedronate (Actonel), and zoledronic acid (Reclast) were first introduced in the mid-1990s, they’ve become a staple of osteoporosis treatment. Yet an FDA review recently published in The New England Journal of Medicine questions whether there’s any benefit to staying on these drugs long-term—especially considering their potential for side effects. A report released today in the Archives of Internal Medicine highlights one of those side effects, linking bisphosphonate use to a higher risk of unusual fractures in the femur (thighbone). If you’ve been taking bisphosphonates long-term, you may be wondering, “What now?” If you’ve been taking bisphosphonates for less than five years you probably don’t need to change what you’re doing. But if you’ve been on these drugs for more than five years, talk to your doctor about whether it’s worth continuing.