Harvard Health Blog
Read posts from experts at Harvard Health Publishing covering a variety of health topics and perspectives on medical news.
Lipitor, the blockbuster cholesterol-lowering drug, is now being sold as a less-expensive generic. Several other best-selling prescription drugs are set to lose patent protection this year, including Actos, a diabetes drug; Plavix, which helps prevent heart attacks and strokes; and Singulair, an important asthma drug. Although the lower price is great, some people worry that changing from a brand-name drugs to a “no-name” generic one might be risky. Not so, says Dr. Anthony Komaroff, editor in chief of the Harvard Health Letter. In the newsletter’s February 2012 issue, he tackles the brand-versus-generic issue. The FDA is legally required to determine that generic products are “bioequivalent” to brand-name drugs, which means that they produce similar blood concentrations of the same chemical. The vast majority of studies show that generic versions are just as safe and effective as their brand-name counterparts.
Resveratrol is a compound that various plants make to fight off bacteria, fungi, and other microbial attackers, or to withstand drought or lack of nutrients. It has been found in red and purple grapes, blueberries, cranberries, mulberries, lingonberries, peanuts, and pistachios. Resveratrol is also abundant in the roots of Japanese knotweed, a plant that has become a hard-to-eradicate invader in the United States.
Back in 1994, the Dietary Supplement Health and Education Act (DSHEA) allowed companies to sell dietary supplements with established ingredients (meaning those that had been sold in the United States before 1994) without any evidence that they are effective or safe. Manufacturers are supposed to give the FDA evidence that a new ingredient should be safe, but this aspect of the law hasn’t been enforced, writes Harvard Medical School’s Dr. Pieter A. Cohen in a commentary in the New England Journal of Medicine. Compare this hands-off approach with the strict rules and regulations for drugs. Last July, the FDA proposed some rules to help it test new dietary supplements. This is a good first step, but the FDA’s plan doesn’t go far enough, argues Dr. Cohen.
Eating disorders don’t afflict only adolescents and young women, but plague older women, too, and may be shrouded in even greater shame and secrecy. Many women don’t seek help, especially if they fear being forced to gain weight or stigmatized as having a “teenager’s disease.” As reported in the February 2012 Harvard Women’s Health Watch, clinicians are reporting an upswing in requests from older women for help with eating disorders. For some of these women, the problem is new; others have struggled with anorexia, bulimia, binge eating, or another eating disorder for decades. Eating problems at midlife and beyond stem from a variety of causes, ranging from grief and divorce to illness, shifting priorities, and heightened awareness of an aging body.
If you want to have a healthy heart in your senior years, take care of it while you’re young. In a large study, researchers from Northwestern University found that a 45-year-old man who had normal blood pressure and cholesterol levels, who didn’t smoke, and who didn’t have diabetes had just a 1.4% chance of having a heart attack or stroke during the rest of his life. Having one major risk factor boosted the risk 20-fold. The results were similar for men and women, blacks and whites. Lead researcher Donald Lloyd-Jones said that making it to middle age with no heart disease risk factors is like “the fountain of youth for your heart.”
Among doctors, there is some controversy over whether or not to use email to communicate with patients. The Wall Street Journal offered a peek into the controversy by asking two prominent doctors to write about why they do, and don’t, use email to communicate with their patients. Writing in favor of email was Dr. Joseph C. Kvedar, a dermatologist and founder of the Center for Connected Health, a Harvard-affiliated organization that aims to move health care from the hospital and doctor’s office into the day-to-day lives of people who need help. Taking the opposite side was Dr. Sam Bierstock, an ophthalmologist who is now the president of Champions in Healthcare, an information technology consulting group. Both doctors make good points making me think that, at least for a while, the use of email will probably come down to personal preference, for doctors and the rest of us.
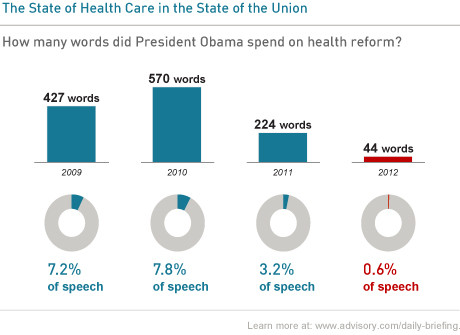
During last night’s State of the Union address, President Obama spent just 44 words on health reform. That’s far fewer than he’s used in the past. Although health care reform may not be a hot issue right now, it is still something that affects us all. What would you have wanted President Obama to have said about it in the State of the Union address?
Many people have trouble quitting smoking even after learning they have cancer, according to a new study from Harvard-affiliated Massachusetts General Hospital. Five months after learning they had cancer, just over one-third (37%) of smokers diagnosed with lung cancer and two-thirds (66%) of those with colorectal cancer were still smoking. The results underscore how difficult it can be to quit smoking. A diagnosis of cancer can be a powerful motivator, but it isn’t always enough—extra help is often needed to quit. Kicking a smoking habit is good for health anytime. It is even more important after a diagnosis of cancer.
The bone-thinning condition known as osteoporosis can be a big problem for older people. That’s why older folks are urged to have their bones checked with a test that measures bone density. Exactly how often to have the test hasn’t yet been set. By following 5,000 older women for almost 17 years, researchers found that the timing of the next bone mineral test should depend on the result of the current one. People who get a normal result can wait 15 years, those with moderate osteopenia should have the test every five years, while those with severe osteopenia should have it every year.
By the year 2050, experts estimate that 16 million Americans will be living with this Alzheimer’s disease. In an effort to head off the explosion, President Obama has signed into law the National Alzheimer’s Project Act. This ambitious project aims to attack Alzheimer’s disease by improving early diagnosis, finding effective prevention and treatment strategies, providing better support for family caregivers, and more. A newly released draft of the project, which a panel of experts is reviewing this week, sets a 2025 deadline for achieving these and other goals. One big drawback—the act doesn’t provide concrete details about how to fund the research and implementation efforts needed to meet the goals.
It is normal for children at some points in their development to be concerned about sameness and symmetry and having things perfect. But when such beliefs or behaviors become all-consuming and start interfering with school, home life, or recreational activities, the problem may be obsessive-compulsive disorder (OCD). Obsessions are irrational thoughts, images, and impulses that a person feels as unrealistic, intrusive, and unwanted. To relieve the anxiety caused by these obsessions, a youth may engage in compulsive rituals. Two main types of treatment are used to help youths better manage OCD: a form of talk therapy known as cognitive behavioral therapy, and medication. The ideal approach is to try cognitive behavioral therapy before turning to medication.
A bold initiative called Million Hearts aims to prevent one million heart attacks and strokes from happening over the next five years. As explained in the Harvard Heart Letter, the initiative is spearheaded by the federal Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services. Its main focus is to encourage more widespread and appropriate use of simple, effective, and inexpensive heart-protecting actions, dubbed the ABCS. These include taking daily low-dose Aspirin, if prescribed; managing Blood pressure and Cholesterol levels; quitting Smoking. The Harvard Heart Letter adds D for Diet and E for Exercise.
Most store-bought muffins deliver the same wallop of highly processed flour and sugar as donuts. Low-fat versions may actually be worse, since they contain extra sugar and salt. To restore the muffin to its rightful place as a healthy breakfast or snack option, chefs and dietitians from the Culinary Institute of America worked on a muffin makeover with nutrition experts from the Harvard School of Public Health (HSPH). They created recipes for five muffins: blueberry, cranberry orange, jalapeno cheddar corn, lemon chickpea, and banana nut. The team replaced half of the white flour with whole wheat or other whole-grain flours, used heart-healthy oils in place of some or all of the butter, added nuts when possible, and cut the size of the muffins.
What is it that lets some people live to age 100 and beyond? A new study from the ongoing New England Centenarian Study suggests that protective genes may make a big contribution.
The U.S. Food and Drug Administration has ruled that farmers must limit the use of antibiotics called cephalosporins to prevent infections in seemingly healthy cows, pigs, chicken, and turkeys. According to the FDA, 24.6 million pounds of antibiotics are used each year in cattle, pigs, chickens, and turkeys purely for the sake of prevention. This practice has contributed to the development of antibiotic-resistant bacteria, which are a growing threat to human health. Doctors often prescribe cephalosporins to stop common infections such as pneumonia and urinary tract infections. They are also used before surgery. Unfortunately, more and more infections are resistant to cephalosporins. Doctors are being asked to prescribe antibiotics only when they are most needed. Farmers should do the same thing. Otherwise, antibiotics lose their power. Bacteria strains become drug-resistant. And people suffer.
Everyone has moments of forgetfulness—misplaced keys, a forgotten errand, the name of that movie you want to recommend but can’t get off the tip of your tongue. A certain amount of forgetfulness seems to be a normal byproduct of aging. But how do you know is forgetfulness signals something more serious, like Alzheimer’s disease or another form of dementia? According to “A Guide to Alzheimer’s Disease,” an updated Special Health Report from Harvard Medical School, by exploring several questions you may be able to get a clearer sense of normal versus worrisome forgetfulness: Is my loved one worried about the memory loss? Is he or she getting lost in familiar territory? Are word-finding problems common? Is your loved one losing the ability to socialize, or interest in it?
During a recent check-up, my doctor snuck a look at her phone a couple times. I don’t think it had anything to do with my health or care, so it was mildly annoying—but I didn’t say anything. After reading a report about a man who almost died because of a doctor’s “multitasking mishap,” next time I’ll speak up. But new research suggests some big downsides to multitasking. According to the authors of Organize Your Mind, Organize Your Life, a new book from Harvard Health Publishing, multitasking increases the chances of making mistakes and missing important information and cues. Instead try set shifting. This means consciously and completely shifting your attention from one task to the next, and focusing on the task at hand.
For many years, nutrition research focused on the benefits and risks of single nutrients, such as cholesterol, saturated fat, and antioxidants. Today, many researchers are exploring the health effects of foods and eating patterns, acknowledging that there are many important interactions within and among nutrients in the foods we eat. The result is a better understanding of what makes up a healthy eating plan. The January 2012 issue of the Harvard Women’s Health Watch offers 12 ways to break old dietary habits and build new ones. These include eating breakfast, piling on the fruits and vegetables, choosing healthy fats, replacing refined grains with whole grains, and eating mindfully.
Although short-term studies suggest that switching from sugar to calorie-free sweeteners can help people lose weight, the December 2011 Harvard Health Letter explores the possibility that it may actually promote weight gain. Use of super-sweet artificial sweeteners may desensitize users to sweetness. Healthful foods like fruits and vegetables may become unappetizing by comparison. As a result, the overall quality of the diet may decline. The calories removed from the diet by the sugar-for-sweetener swap may sneak back in, in the form of refined carbohydrates and low-quality fats. Another concern is that artificial sweeteners could cause weight gain by directly stimulating the development of new fat cells.
Family and togetherness are key themes for the holidays. That can make the holidays awfully difficult for people who are grieving the loss of a loved one. My father passed away a month before the holidays. We still shared presents, ate large meals, visited with friends, even sang carols—but it was all pretty subdued.
New guidelines for from the American Academy of Pediatrics recommend that all kids between the ages of 9 and 11 have their LDL (bad) cholesterol levels checked. The rationale is that atherosclerosis (the fatty gunk in arteries that causes heart attacks, strokes, and other serious problems) starts during youth. Atherosclerosis is fed by high LDL. The guidelines aren’t aimed at getting kids to take cholesterol-lowering statins. Instead, they are about getting kids, their parents, and their doctors to talk about making healthy lifestyle choices. The hope is that more doctor time spent coaching and counseling now will mean less time treating cardiovascular disease later.
As paper medical records give way to electronic health records, it is becoming increasingly possible to view your medical history. Yet experts are debating whether the electronic health record should include the notes that doctors make in them. The Open Notes project is designed to test the consequences of giving patients access to doctors’ notes. Results of a survey of the expectations that doctors and patients have for note sharing, reported in the Annals of Internal Medicine, suggest that while physicians are generally optimistic about doing this, many believe it could cause patients to worry or generate unnecessary questions. Patients who filled out the survey thought that seeing their doctor’s notes would provide a clearer understanding of their medical condition, improve self-care, and give them a greater sense of control.
“Limit salt” has been a key part of dietary advice for decades. Once aimed at individuals, the FDA is hoping to persuade food companies to cut back on salt added to prepared foods. That’s probably a good idea, since the average American gets more salt—and thus sodium—than needed, most of it from prepared foods. But the question of how low we should go with sodium hasn’t been answered. Two studies suggest that getting too little sodium could pose problems, just as eating too much does. Trials to determine the safest range for sodium aren’t in the offing. What to do in the interim? Aiming for the recommended target of 2,300 milligrams per day from all sources is probably good for most people.